Date: 22 Thursday 2024 @ 6:30pm
Location: Moss Valley Medical Practice
| In attendance: | Apologies: | Invited in addition: |
| Glyn Jones – Chair Margaret Askham Shelley Hinson Adrian Hubbard John Hutchinson Wendy Jones Helen Lane Mary Milner John Needham Dr L Moss – GP Partner [LM] Carole Mason – Practice Business Manager [CMA] | Pat Boyle Evelyn Kirby Mike Kirby Andrew Loughran | Sarah Curl – Pharmacist (Peak Pharmacy Dronfield) Kay Howarth – Manager (Peak Pharmacy Dronfield) |
Practice Update
CMA shared the following practice update with members.
New Starters
Tracey Cocking – Cleaner (Moss Valley)
Joanne Stanton – Assistant Practice Manager (Moss Valley)
Changes
Dr Tom Martin is now Clinical Director for the PCN
Leavers
Kay Straker – Patient Administrator at Moss Valley (retirement)
Kathryn Collier – Nurse at Gosforth Valley (retirement)
Vacancies
New Services
New Initiatives
Vaccination engagement campaign
Events
Challenges
Ongoing Junior Doctors Strikes
Winter pressures
Wins
PCN News
Change of Practice Manager at The Springs Medical Centre
Home Visiting Team will be playing a bigger role in support Care Home residents across the PRC practices
CMA added the following detail:
Joanne Stanton
Joanne Stanton and colleagues at Moss Valley were looking forward to Joanne joining the team as there had been a gap of 3-months between the previous Assistant Practice Manager leaving and Joanne joining. This was because of an issue following the first round of interviews and the practice being let down by the candidate who had been offered the post.
In the interim period Carol Mycock (Assistant Practice Manager at Gosforth) and Charlotte Helley (Finance Officer) had been an amazing support and she was very grateful to them both.
Retirements
CMA outlined how, between them, the three colleagues who were retiring had completed 62 years’ service for The Valleys. Arrangements were in place to celebrate their contributions. Members of the PPG reflected on their positive experience of colleagues who were retiring, particularly Kathryn Collier who many of Gosforth Valley representatives regularly saw.
CMA said that she felt that staff retention had improved, and whilst it was sad to see colleagues leave, it was a more positive position for the partnership where this was because of retirement or promotion.
Patient Administration Vacancy
CMA said that as this is a maternity cover and a short-term appointment it may be more challenging to recruit to, so she would be grateful if the PPG could spread the word and let her know of anyone who may be interested.
Vaccination Engagement Campaign
CMA explained that as a PCN, all practices had accessed additional funding to try and encourage people who hadn’t take up their offer of a vaccine (in this instance, Covid), to have it. The work also helped us to understand the reasons why patients hadn’t or didn’t want to engage.
The PCN had collectively contacted almost 600 people as part of this project, with 10% of those contacted taking up the offer of a vaccine. The ICB had been impressed with the work the PCN had done in this area, and as a result, a similar campaign with a focus on measles, would be taking place.
Star of the Month!
In line with the practice’s core value of celebrating success, CMA advised that at the monthly practice meetings, staff, or groups of staff, were being nominated and rewarded for their contributions. CMA suggested that members of the PPG may want to consider, where they experienced excellent service, or a had a positive experience, nominating someone, or a team, for a ‘Star of the Month’ PPG award. A member referenced their recent experience with a colleague in the nurse/HCA team, and how at ease they had been made to feel when attending the practice as a result of a serious illness.
Action: CMA to check which member of staff it was and include in awards as a PPG nomination for March.
Spring Booster Campaign for Covid
CMA said that the provisional date for the vaccination clinic was 23 April 2024. The Chair confirmed he was on holiday so would be unable to support the Spring campaign, but encouraged other members to do so where they could.
Percentage of GP appointments available at The Valleys
CMA said she was proud that recent statistics released about the proportion of appointments across practices in the area showed that The Valleys were offering almost 20% more GP appointments than others. This wasn’t to devalue other types of clinicians, who were often best placed to treat and support a whole range of conditions, but it did show that The Valleys took their values in terms of preserving the core values of general practice, seriously.
In addition to the information shared, Dr Moss informed members that on 2 March 2024 she would be made a Fellow of the Royal College of General Practitioners, after being nominated by colleagues. All present at the meeting congratulated Dr Moss on the fantastic achievement.
Members asked the following questions in response to the update:
Q: Had the practice found that cases of influenza had been more significant than Covid over the winter this year?
A: Certainly, that is my experience [Dr Moss].
Discussion also took place about the extent to which anti-vaccination messages affected the uptake of immunisations, specifically MMR.
Q&A Session with Sarah Curl (Pharmacist) and Kay Howarth (Manager) from Peak Pharmacy at Dronfield
The Chair thanked Sarah [SC] and Kay [KH] for attending the meeting and invited them to address the group.
SC informed members about the way the funding for pharmacies was changing, and how Peak Pharmacy was investing significant amounts of money into meeting the new challenge. SC explained that the Government believe that pharmacies had a role to play in supporting primary care, and that this was being delivered through the new ‘Pharmacy First’ model. SC shared a document that outlined the service with members.
It was explained that Pharmacy First had already been operating in some guise, with GPs being able to refer into the service as well as patient’s self-referring. This had proven to be particularly useful at weekends and on bank holidays when GPs were closed.
The previous offer had now been extended to encompass a new clinical consultation pathway, and SC explained how this worked and the conditions it covered.
SC said that they recognised that through the clinical consultation pathway, it was likely that there would sometimes be a need to prescribe antibiotics, and this wasn’t something that they took lightly. SC reassured members that the service was very specific in terms of who would be targeted, and the work of the pharmacies would be audited. They had also received additional training to be able to deliver the service.
The Chair opened the floor to questions and/or comments from members and practice representatives:
Q: Can any patient walk into any pharmacy?
A: Yes. Patients may initially find little pockets where pharmacies haven’t yet achieved the competencies to deliver the programme, but this would be rear. Even when there was locum cover in place, patients should find that locums were trained to deliver the service.
Q: Where are the clinical findings recorded?
A: Where systems were integrated with the pharmacy system, the findings would be shared with practices in this way. Where they weren’t, pharmacies were obliged to send a paper copy to the patient’s GP practice. This was still a work in progress and the service had been a quick turnaround, from its inception in May 2023, to rollout at the start of February. The PGDs that underpinned the service were very specific, detailed, and wordy, so there should be confidence in the work that the pharmacies were undertaken.
Q: If the pharmacist is dealing with consultations, how will dispensing be affected?
A: This is an example of how the organisation is adapting to the change in funding. Dispensing could be done using AI, with very little human intervention. Peak Pharmacy had invested in a ‘hub and spoke’ dispensing model which meant that the majority of prescriptions were sent to a central location to be processed by a machine and sent back to branch to dispense to patients. Therefore, a significant amount of the dispensing moving forward would be done offsite.
All companies needed to adapt to the new funding model; the sector had already lost Lloyds, and this proved that no one was too big to fail. The intention was to move much of the traditional/routine dispensing out, and retain the acute dispensing. By doing this, it would allow time to focus on patient consultation.
Not all prescriptions would go to ‘hub and spoke’, for example, glass bottled prescriptions, acute, walk-in and same-day prescriptions.
Q: Will you still need to go into the pharmacy to order your batch prescription?
A: You can also request this over the phone. Patients should be aware that in the first instance, while the new ‘hub and spoke’ model is being embedded, prescription turnaround times may be a little longer. There were 140 Peak Pharmacies to bring online with this nationally, and it was important the rollout was done at a sensible pace. The pharmacies would be sharing the timeline with patients to help them to understand the process. Timeframes would improve, and the service would become quicker, as time went on.
Q: How would the new system support people who potentially need more support? For example, those who may be elderly or infirm and may struggle with the concept of new technologies?
A: By educating the people who can access the service in different ways, capacity would be created to support the people who needed more traditional support.
Q: If the batch is processed offsite, do patients still request this in the same way?
A: Yes.
Q: Will this affect same-day requests?
A: No – these will still be dealt with in-house.
Q: [From SC to practice representatives] what do GPs think about the introduction of the service?
A: There is recognition that we need to embrace this new way of working, but there are reservations about the level of training and the potential over-prescribing of some medications.
Questions paused for discussion:
SC said that the guidelines were very clear about where the line was for what pharmacies could deal with, and what needed to go back to GPs. They had met with a partner from The Valleys to agree the process for referring into the practice. They were very aware of the antibiotics issue, and the implication of over-prescribing, and took this responsibility very seriously – the procedures were very specific.
LM explained that many GPs were under pressure and worked hard not to create a reliance on medication, and she would hate the UK to mirror other countries where antibiotics or similar medication were available easily over the counter.
CMA said that for this to truly work and have a positive impact on capacity at practice level, it was also important that patients were only dealt with once. If patients were triaged by the GP into the Pharmacy First service, but these patients were then sent back as the pharmacists couldn’t deal with them, then the service was likely to fail, and the service would become counter-productive.
Questions resumed:
Q: What happens if a patient refuses to give their GP details, can they still be treated?
A: Pharmacy can still treat them; the pharmacy must have consent to share information back to the GP. Where a patient didn’t give consent, the pharmacist would look to understand the underlying reasons for this.
Q: What capacity can pharmacies manage and how many are they averaging currently?
A: It’s difficult to say now, currently averaging one per day. Patients don’t currently get given an appointment time, but they may need to introduce this if referrals increase. There is no maximum/minimum length for the consultations.
Q: Can you see a time when you’ll be over capacity, and if you were, how would you manage this, because it would be unfortunate if referrals were turned down or referred into general practice due to a lack of capacity?
A: If capacity did become an issue, the fallback would be to use other pharmacy branches in the chain and not to refer back or refuse consultations.
Q: One of the main concerns is patients seeing this as an opportunity to get antibiotics, from pharmacies easily and if there is the potential that this is financially beneficial from the perspective of selling the drugs and for completing the consultation – how will this be managed?
A: The payment for consultation is not reliant on a prescribed drug outcome at the end. The financial renumeration is the same if self-care advice is given.
Q: Is there a risk that, by giving patients another, potentially quicker route, to access medical professionals, we lower the threshold in terms of self-care?
A: The pharmacy teams appreciate the role they must play in terms of promotion of self-care and building patient resilience, and this will be a key feature of consultations moving forward.
Q: If stock is being moved centrally, how will this affect same-day requests and stock levels at individual sites?
A: This shouldn’t be a problem.
The Chair thanked SC and KH for attending and answering questions and said that it had been a positive and informative session. Members passed on their thanks to Peak Pharmacy at Dronfield and said that the service they receive from the team was impeccable.
SC and KH left the meeting.
Local Update: Acute Respiratory Hubs
The Chair shared an article from Joined Up Care Derbyshire about that stated thousands of additional appointments had been made available. He said that when he had discussed this with CMA, she had explained what this meant at The Valleys.
The Chair invited CMA to go through the information with members, and CMA shared the following slide in response:
Acute Respiratory Infection (ARI) Hubs
What does it mean for us?
PCNs have received a small amount of funding to provide additional ARI Hub appointments.
The inclusion criteria is “…adults and children with acute respiratory symptoms, most likely due to an infection (eg, bacterial, or viral infections including COVID-19, RSV, influenza), who have been identified as requiring face-to-face assessment but not requiring direct hospitalisation”.
In North East Derbyshire PCN, the funding has been divided between each of the 4 practices to deliver their own ARI Hubs. This has given The Valleys an additional 113 ARI Specific same-day, faec-to-face appointments between 1January and 31 March.
Patients won’t necessarily know they’re attending an ARI hub appointment.
There were no questions or further points from members in response to the information.
National Update: Increasing cases of Measles
The Chair invited CMA to share information with members about the national concerns for a Measles outbreak.
In response, CMA went through a short presentation which include extracts of slides Dr Marney had shared with staff at a recent practice meeting:
Increase in Measles Infections
What’s the worry?
Coverage for MMR in UK Has fallen to the lowest level in a decade:
- First dose uptake in 2-year-olds is 89%; second dose uptake in 5-year-olds is 85.5%
- To achieve and maintain measles elimination (and prevent outbreaks) we need 95% uptake with 2 doses of the MMR vaccine by the time children turn 5 years.
- Figures released by the UKHSA show there have been 347 confirmed measles cases since 1 October last year.
- 75% in West Midlands, 13% London and 7% in Yorkshire & Humber, with the majority being in children aged under 10.
What are we doing?
We are considering measles for any patient with fever AND rash AND one of runny nose, cough or conjunctivitis.
Where this is the case, the triaging clinician will check if ANY of the following apply:
- Unvaccinated or partially vaccinated
- Has recently travelled to a area where its circulating
- Has had contact with a confirmed or suspected case
If the decision is that we need to see the patient face-to-face, we will bring them straight from car park to the consulting room, we will wear PPE and we will encourage the patient to wear a mask.
If patient has a suspected case of Measles, we will notify the Health Protection Team and they will arrange testing and deal with contacts.
What we are doing? Vaccination push!
- We are checking the immunization history of every patient, especially for children, new registrations, new migrants, refugees and asylum seekers.
- To protect themselves, and to prevent transmission of measles in health care settings, the vaccination status of any patient-facing staff is being checked, and staff are being encouraged to be vaccinated if they haven’t been.
Members discussed the level of response from the government in respect of what was perceived to be a relatively small outbreak, and wondered if there was a reason for this.
CMA said that the main message to take away, was to promote vaccination as this was the best way to keep everyone safe.
Feedback: New Phone System
The Chair said that the new phone system was now in place, and he had discussed with CMA the potential for members to give feedback, but also for CMA to share data about the volume of calls the practice were dealing with.
The Chair invited feedback from members:
There are a lot of Americanisms on the messages and different voices.
Action: CMA to review phone message.
The Chair invited CMA to go through the data. CMA talked through data which outlined the number of calls that each practice was managing each day, on average:
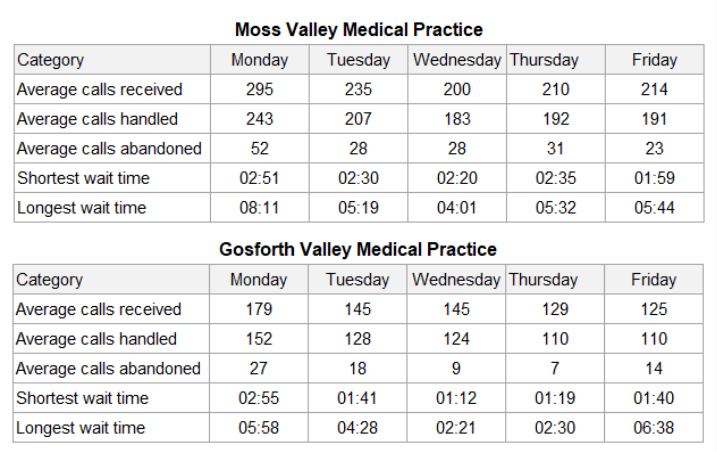
CMA referenced the difference in call volume, wait time and abandoned calls between the practices and reminded members that Moss Valley held 2/3 of the patient list, and Gosforth 1/3, however the number of staff answering calls at each site was the same.
CMA said that the initial reaction is that more staff need to be assigned to answering phones at Moss Valley, however, phone calls were only a small part of the administrative duties of the reception team, and this wasn’t necessarily the right place to increase spend. CMA suggested that the better way forward was to look at how the practice could support patients to use other routes to achieve what they needed.
Using the example of appointments, CMA explained how, quite often, patient perception was that by calling the practice a patient could get an appointment quicker than they could by filling in the form online. CMA said that the route to an appointment was the same, regardless of whether a patient called the practice, or filled the form in directly, with the only difference being that when a patient called up, the receptionist answering the phone filled the form in on behalf of the patient.
CMA shared the following diagram with members to illustrate her point

CMA attempted to demonstrate how the AccuRx appointment request worked, but as it was after 8:00pm, was unable to do this (AccuRx appointment requests online are only available between 08:00 and 20:00).
Members who had used the online appointment request form said that they found it brilliant, time-saving, and effective. Members who hadn’t used it said that they hadn’t realised the journey was the same for phoning in and using the online template.
CMA advised that the link could be accessed via the practice website, or direct: https://florey.accurx.com/p/C81002. It was possible to save this to phones, or desktops for ease of use, and the ‘admin’ function also allowed patients to request things like sick notes.
Members who hadn’t used AccuRx said that they were going to give it a try.
CMA said that the practice recognised that this wasn’t for everyone, and there would be patients who, for whatever reason, would need to phone the practice, but by helping everyone to access the different functions of the practice in the way that was right for them, we could hopefully free up the phone lines and improve access.
CMA apologised that she hadn’t been able to demonstrate AccuRx and said that she was putting a video together about this which she would share with members instead.
Members asked if the video would go on the website, CMA said it would, but she would appreciate their feedback first.
ACTION: CMA to share video with members of the PPG for feedback before adding this to website.
Any other business
The Chair invited members and representatives of the practice to share any other brief items for discussion:
- Website
On the ‘News’ section, the ‘BBC Health’ links are working, but the ‘NHS Choices’ links aren’t.
ACTION: CMA to review and amend as appropriate. - Screen in waiting room at Moss Valley
There is a page that refers to NHS Scotland, and some of the pages are blurry.
ACTION: CMA to review and amend as appropriate. - DHU
DHU contract for 111 out of hours service has been renewed for a further 2-years. Members who had used the service commented that they had found this to be positive. - PPG Membership
The Chair raised the need to look at increasing membership. After discussion it was agreed that the PPG would look to attend and promote its work when the Spring Covid clinics were taking place.
Date of next meetings
The Chair thanked everyone for attending, and for their contributions, and confirmed that the next meeting would be held on Thursday 16 May 2024 from 18:30 at Gosforth Valley.
