Date: 18 July 2024 @ 6:30pm
Venue: Moss Valley Medical Practice
Attendance & Apologies received
| In attendance: | Apologies: | Invited in addition: |
| Glyn Jones – Chair Margaret Askham Adrian Hubbard John Hutchinson Wendy Jones Helen Lane Andrew Loughran Mary Milner John Needham Carole Mason – Practice Business Manager [CMA] Dr Louise Moss – GP Partner [LM] | Shelley Hinson Bradley Mee-Evans | Dr Beth Marney – GP Partner [BM] |
Practice Update
CMA shared the following practice update with members.
New Staff
Dr Steven Tao at Moss Valley
Changes
Rebecca Forshaw – Patient Administration Team Leader at Gosforth Valley
Leavers
Goodbye to GP Registrars
- Dr Ben Cumberland [Gosforth Valley]
- Dr Arthur Joustra [Moss Valley]
- Dr Alex Knapton [Moss Valley]
- Dr Talha Syed [Gosforth Valley]
- Dr Ramish Tariq [Gosforth Valley]
Vacancies
New Initiatives
Management Structure – Moving to a more cross-site management team with defined responsibilities.
Change to Friends and Family tests
Events
Challenges
Website
Staff annual leave
North East Derbyshire Primary Care Network (PCN) News
New Vacancies in the Home Visiting Team
New role under the Additional Roles Reimbursement Scheme (ARRS)
Visit from Chris Clayton – Chief Executive of the ICB (Joined Up Care Derbyshire)
CMA added the following detail:
Cheryl Harding
A vacancy had arisen following internal promotions for colleagues and Cheryl had started with The Valleys, at Gosforth, at the beginning of July. Cheryl had made an excellent start. Members endorsed this view and shared their positive experience of the interactions they had had with Cheryl over the previous 2 weeks.
Action: CMA to share feedback with staff member.
Dr Steven Tao
Members and patients may remember from his previous time at the practice, Dr Steven Tao has returned to cover one day a week (Thursdays) for Dr Doole, who has given birth to a healthy baby boy!
Nicola Mallows and Rebecca Forshaw
Nicola Mallows and Rebecca Forshaw had been promoted to the posts of Assistant Practice Manager (following retirement) and Patient Administration Team Leader respectively.
CMA outlined the commitment of the Partnership to develop future leaders within the organisation, and that it was excellent to see colleagues wanting to progress. She added that the Valleys had a brilliant team of staff and would be working with those who had expressed an interest in moving to promoted posts in the future.
Goodbye to GP Registrars
A member shared lovely feedback about Dr Cumberland and the support he had given to a relative, in terms of care, proactively and going above and beyond.
Action: CMA to share feedback with staff member.
A member shared their frustration about Registrars who train in the UK, but then move abroad to practice. They asked if the NHS had thought of building in fines, or a clause about repayment of monies if they did this within the first 2-years for example. Dr Moss said that the bigger problem was that terms and conditions for doctors in the UK were less favourable than in other countries, and this probably needed to be the focus, rather than penalising those that moved abroad.
It was also recognised that it was very expensive to train, and doctors qualified with a huge burden of debt, as did professionals in other sectors.
Practice Nurse Vacancy
CMA explained that cover for Connie Tracey would begin around October. As Connie worked cross-site Debbie Dujon and Emma Brealy would both be increasing their hours during Connie’s absence, and the hours that couldn’t be covered internally (2.5 days) would be advertised externally.
CMA confirmed that Debbie would be covering at Gosforth, Emma at Moss Valley, and Kim Longstaffe (nurse) would be spending 1 day a week at Gosforth Valley, rather than Moss Valley while Connie was off work. The new nurse would be based predominantly at Moss Valley.
Management structure
CMA outlined that with the changes to the management team recently, there was opportunity to move to a cross-site structure, so while the Assistant Practice Managers would retain operational responsibility for each practice, they would then pick up a cross-site focus. Joanne Stanton (Assistant Practice Manager at Moss Valley) would focus on systems and structures including rotas, and Nicola Mallows (Assistant Practice Manager at Gosforth Valley) would have a ‘people’ focus, leading on trainees, staff training and appraisal for example.
CMA said she was excited by the change and felt that this gave the partnership opportunity to continue to improve the consistency of experience for patients across the partnership, as well as create efficiencies and develop expertise.
Covid vaccine clinics
CMA confirmed that clinics will be taking place at some point during the first 2 weeks in October. Discussed the new RSV vaccine for 75- to 79-year-olds that targeted respiratory syncytial virus (RSV).
CMA explained that this was relatively new news and the practice still needed to understand the requirements of how the vaccine could be deployed, but it was likely that, if we could, we would look to co-administer this alongside covid and flu.
Patients treating our staff with respect
CMA said that the staff they had at The Valleys worked incredibly hard and were really committed to providing the highest levels of service to patients.
Unfortunately, recently, there had been increasing examples of staff not being treated with respect. This ranged from intimidating behaviour in reception and with clinicians, to a previous local councillor allegedly being derogatory to patients about one of the practices, to patients calling staff names to other clinicians. This was not okay and would not be tolerated.
Members were disappointed to hear this but reflected that they felt this was a more common occurrence in society generally. Members asked what the partnership were doing, if anything, about this. CMA advised that they would be reviewing their signage in waiting rooms at both practices, upskilling staff in terms of actions to take to challenge/manage this type of behaviour when it occurred, and they would be following up any instances directly with the patient concerned.
Website
The Partnership recognised that the website was key to improving access to appointments for patients, and to reducing the volume of calls both practices received. As a result, it was working on its website currently and members may have noticed some changes. Members asked for a live demonstration of where to go to book appointments, because they had previously felt that this wasn’t clear, which CMA facilitated.
Website: Appointments
Staff annual leave
As with any organisation, the school holidays saw lots of staff taking annual leave, which did mean at times the wait on the phones would be longer, as the practices may be down to only 3 people answering calls across the two sites (on average the practices handled around 500 calls per day), or that the wait for routine appointments may be longer. CMA recognised that this was no different to any other organisation, and unfortunately there wasn’t the funding, or the staff availability, to cover these absences. She apologised for any impact that patients felt as a result of this.
There were no additional questions asked.
Presentation and Q&A Session: Research
The Chair welcomed Dr Beth Marney (BM) to the meeting and invited her to introduce herself to members. BM advised that she was a GP at The Valleys, and one of the Partners, and had recently been appointed as the Research Champion for Derbyshire.
BM passed on the apologies of Bradley Mee-Evans (BE), who was the Primary Care Research Facilitator for the National Institute for Health and Care Research and explained that the absence was due to a family illness.
BM informed members that she would go through the slides BE had intended to present, and then talk more about why the partnership had chosen to get involved in research.
The presentation delivered on behalf of BE provided an overview of research and some of the projects that were currently open and available for patients to sign up to.
BM outlined to members that The Valleys were involved in research for several reasons:
- Currently most research happened in secondary care.
- The burden of ill health lies in the community.
- Only the most severe needed hospital care and therefore represented only a small minority.
- Primary care as a research setting, is accessible to almost all the population.
BM set down the challenges to research:
- Areas with the highest burden of disease have the lowest numbers of patients taking part in research.
- This means that diseases which are more common among deprived communities are being studied in healthier populations.
- This matters because findings from healthier populations may not hold true in communities which face greater challenges to health and wellbeing. It is also unjust as publicly-funded research should be accessible to all.
BM explained that the role of the partnership was delivery of research opportunities, and they weren’t involved in research design. She then invited thoughts from the group, together with any comments, feedback and questions and/or questions, with a particular focus on the following points:
- How did members feel about the practice being research active?
- Had any members been invited to participate in any studies?
- How did members feel about receiving the invitation?
- What did members think about the mode of communication (for example, text not letter)?
- Did members feel text fatigue and if so, could they suggest a better mode of communication?
- What areas of research were important to members?
[Q=Question; A=Answer; C=Comment]
C: The poster about the MELS research project at Gosforth Valley has the wrong number on it; when you call it doesn’t connect.
Action: BM to contact research provider as all promotional materials are sent direct from them.
Q: Is doing research detrimental to the number of appointments the practice can offer?
A: BM has a small amount of time built into rotas to facilitate research, as does Debbie Dujon (Research Nurse), but this equated to between 30-minutes to 1-hour per week. The ‘Research Champion’ role was funded separately and completed by BM primarily in her own time.
Q: Are patients screened before invitations are sent?
A: Yes, based on a broad criterion depending upon the requirements of the study. For example, patients over 18 with mental capacity and who consent to receiving text messages. Patients aren’t however, screened on an individual basis and sometimes it means that we get it wrong, for example, an end-of-life patient may receive a text. We have taken the view not to screen individually as those patients have an entitlement to take part in research too, and we risk restricting participation and the authenticity of the results if we include too big of a group.
C: Feel that research is essential and akin to having GP Registrars in practice. It is beneficial for the practice, and really beneficial for the patient. An example was given of a study that a member had taken part in focusing on blood pressure, and whether medication was more effective if taken in the morning rather than the evening. The results of the study had helped improve care for the member and others. Another example was given of a study around chronic fatigue syndrome which had identified a link to at least three genetic markers. Would encourage and be supportive of the practice doing as much as it can to support research.
Q: Do you have any control over the quality of the people who provide follow-up for studies? A member took part in a study focusing on gout several years ago and the nurse who came out to see them was not good and they did not want to let them into the house. This experience has put them off taking part in further studies.
A: We tend to deliver recruitment studies, which don’t necessarily have follow-up care in this way and tend to be more time-consuming, require additional funding to backfill and run at a bigger scale. If ever a patient does have concerns about any aspect of a study they are taking part in, we would encourage them to come back to the practice. We may redirect them to the study team, but we would want to know. We work hard to ensure we are only involved in credible studies that are worthwhile and relevant to our patients and local community.
Q: Are the results anonymous or will taking part in a study generate a result or a diagnosis that would be included on a patient’s medical record, and would need subsequently to be declared for insurance purposes?
A: Most of the studies involve collecting anonymised data and the result doesn’t come back to the patient or the practice. Some do, and if you were to receive a diagnosis (for example high blood pressure), this would write back to your record, and you would need to declare this. The way in which the data is handled should be set down clearly at the start, and you usually have to sign to say you agree to your data being dealt with in the way that’s set down. If you have any questions prior to taking part in a research project, we’d encourage you to get in touch.
Q: A discussion point was about the areas of research patients would like the practice to get involved in; if patients don’t know what research is available, it’s difficult to know what they can take part in, should we be sending out texts asking patients to express an interest?
A: Currently the practice take part in around five carefully chosen research projects each year. The ones we chose not to take part in are usually irrelevant to our patient population, poorly thought through, or time intensive. We don’t have the time or resources to do every project. Patients who are eligible to take part in the ones we run will receive a text invitation, but it may be useful for the partnership to potentially include something on the website where patients could sign up to other research projects that aren’t being run by the practice.
Action: CMA to add information to the website about how patients can sign up for other research projects.
Q: Is there any potential for patients being asked to be involved in scam research projects, and receiving illegitimate texts?
A: Not that we’re aware of, any text sent from the practice is because of a legitimate research project. However, we know the fear of scams and fraudulent attempts to obtain patient data is a barrier to some patients signing up and taking part.
Q: What do members think about receiving text messages?
Q: What about emails? [Member]
A: The practices don’t tend to have the same volume of email addresses recorded for patients, as they do mobile numbers, or the mechanism to send email on bulk, which is why we tend to go for texts.
Q: Do I call in to the surgery if I want to take part?
A: Each research project is open to patients who meet specific criteria. If you receive a text message, you’ve been identified as eligible to take part, so you can respond by following the link. We can also look how we can improve the quality of the information on the website to promote our research work.
Q: The best way to improve uptake is through one-to-one conversations, is there any scope for clinicians to mention it to patients at the end of their appointment if there is time?
A: This isn’t always consistent and is easy to forget. Suggest this might lend itself well to an event such as Covid/Flu vaccination days.
Action: CMA to follow up with Adrian Hubbard, Helen Lane and John Needham, who all expressed an interest in supporting with this.
C: A member expressed an interest in taking part in any research studies for long-term amputees.
Q: Is the majority of research NIHR (National Institute for Health and Care Research) led, or sponsor led? (Member offered to provide GCP (Good Clinical Practice) training for free).
A: At the moment we don’t tend to do any sponsor led research as this tends to be too time intensive. Action: Offer of free GCP (Good Clinical Practice) training from a member – BM to contact them if this is something the practice would like to take up.
Q: From a patient perspective, we’re interested in any studies that look at conditions we have been diagnosed with, but what are the doctors’ views of what research projects are important?
A: Blood pressure, weight loss, any studies that access those patients who are harder to reach, studies that reduce the impact of long-term conditions.
Q: What would be the top 3 studies?
A: 1) Mental health; 2) Vaccination trials; 3) Antibiotic resistance, but then also weight loss, smoking. The Chair thanked BM for her presentation. BM invited members to share any additional thoughts or comments after the meeting with CMA. BM closed by sharing her enthusiasm for the promotion of research by members of the PPG at the vaccination event in October, and that the partnership would continue to look at ways in which they could improve the website.
GP Patient Survey 2024 – Results
The Chair invited CMA to share the results of the 2024 GP Patient Survey.
CMA advised that this was the survey that was managed nationally by NHS England, that was sent to a random selection of patients between January and March. CMA explained that the 2024 survey results were the start of a new series and this meant that trend data for previous years couldn’t accurately be compared. She explained that this was mainly for 2 reasons:
1) The questionnaire had been updated to make sure it reflected how primary care services are delivered and how patients experience them.
2) There had been changes to the survey design which meant there was now an ‘online first’ approach, which was designed to improve response rates and reduce costs.
CMA shared an overview of the results:
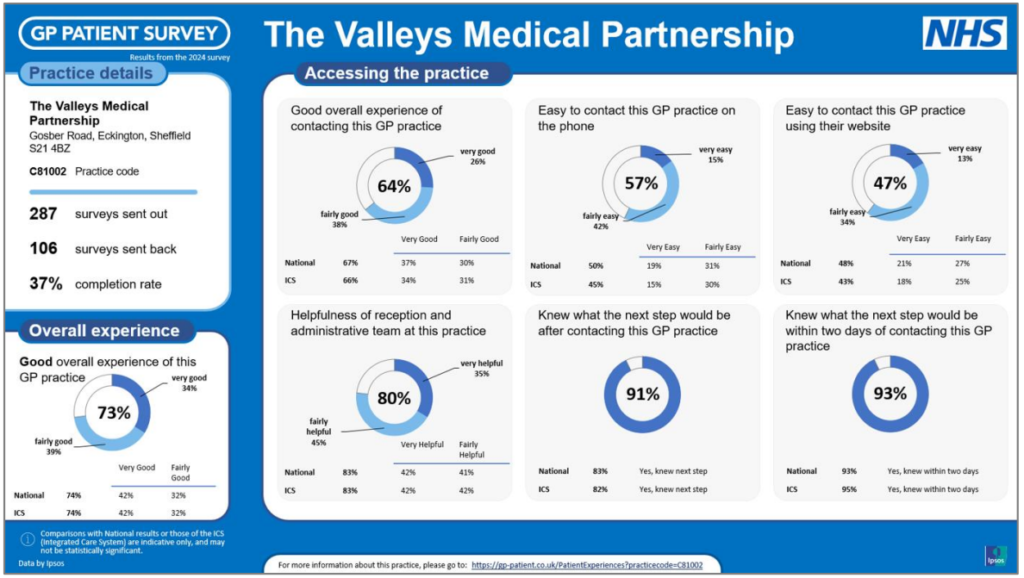
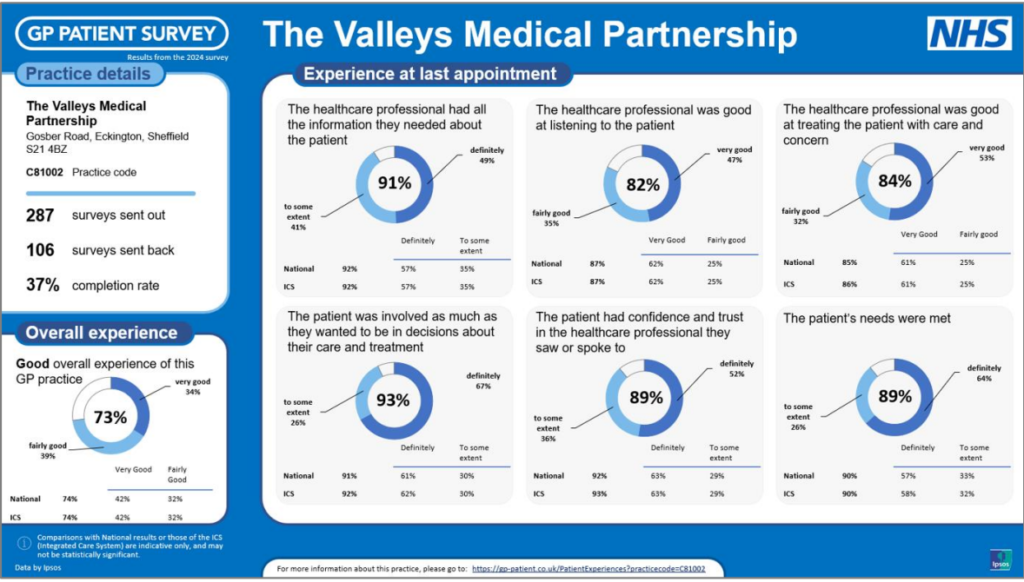
CMA said that whilst there was much to be pleased about, including the number of areas in which the practices were performing above the national average, there was a real drive from the partners and management team, which was also shared by the staff team, to deliver the best possible care for all the patients of The Valleys.
CMA said that it was important to keep the results in context. The response rate for the partnership was 37%, with a total of 106 questionnaires returned, so this was only representative of a relatively small proportion of the 12,400 patients The Valleys served. Nonetheless, it was essential that the results were used to inform areas of development.
The two main things that the survey results had underlined were:
- The ease of access getting through to the practice – the volume of calls into the practice was ever increasing, with around 500 calls being received every day, and often 3 or 4 members of staff across both sites answering the phones.
- The availability of appointments at the time the survey was conducted, which came at a time where the wait for routine appointments was over 2-weeks, and sometimes as long as 4.
CMA advised that, to give the results context, she had prepared a comparison with national results, the results across Derby and Derbyshire (ICB), the other PCN practices and the practices that were closest in terms of location, to Moss Valley and to Gosforth Valley. Members reviewed the comparison data; the results for The Valleys placed them in the middle (not the worst but not the highest performing). CMA advised that the ambition of The Valleys was to be at the top.
CMA asked The Chair if she could move on to the next agenda item, as this was linked, and set out how the practice intended to address the results of the survey.
Access to Appointments
CMA advised that, whilst the results of the GP survey gave a snapshot and overview, it didn’t provide the detail underneath that would help the Partnership to pinpoint what change was needed, and what the barriers were to achieve the change. Because of this, the partnership had chosen to move to a new way of collecting Friends and Family Test data (FFT).
For patients, very little would change. There would still be the link to complete the FFT questionnaire sent by text message after each appointment. The first part of the questionnaire would be the same:
“Thinking about your GP practice overall, how was your experience of our service?” (Response options ranged from “very good” to “very poor”). Patients then had the opportunity to leave a comment. The following aspects had then been added:
– Patients were asked to indicate whether their appointment related to Moss Valley or Gosforth Valley. CMA identified that it had not been possible to break the results down previously and this would be useful given the ongoing commitment to ensure the experience across both practices was consistent.
– Patients were then asked if they had time to answer a few additional questions. For July, and likely August, the focus was how patients had made their appointment, and what the barriers were to making an appointment online.
CMA emphasised that the push to asking patients to make appointments online was not about wanting to stop everyone from calling up, but it was about recognising how we got patients to the right outcome, in the best way for them, via the most efficient and effective route.
CMA outlined that the volume of calls the practice received daily continued to grow. She acknowledged that the wait for calls to be answered some days was significant, with patients waiting almost 20-minutes at really busy times. CMA explained that there wasn’t an infinite pool of funds and the Partnership had to prioritise; whilst it recognised the frustrations of patients, increasing the number of people answering the phone would mean that there were less funds for other aspects of the practices’ work.
CMA advised that if the Partnership could increase the number of patients who access services online rather than via phones, those patients who had no alternative but to contact the practice by phone (for example, because they had no internet, or didn’t know how to), could get through quicker.
Brief discussion took place about the barriers to people accessing the practice’s services online, and from feedback from some local community groups that members were involved in, this quite often, was down to a lack of confidence, misunderstanding, or not knowing how.
CMA said that she would be really happy to come out to any community groups, to help get people set up on the NHS App, and to help people to understand how they can access some of the online services that are available. She confirmed that she was happy to do this at any time, if members felt that a group, they were involved in would appreciate this.
Action: Members to contact CMA if any community group they are involved in would appreciate a demonstration/question and answer session about how to access appointments at the practices.
Members suggested that the upcoming vaccination events might be an ideal opportunity to demonstrate how to, for example, book appointments using the online link, and that the age range of people who attend were possibly the target audience.
Action: Members to work with CMA to look at how this can be incorporated into the upcoming vaccination events.
Dr Moss made reference to the upcoming Wellness event being held in Eckington on 9 August 2024, and suggested that this might be something the practice wanted to be represented at. It would be a good opportunity to meet with patients and members of the community.
Action: CMA to contact organisers to see if this is something we could potentially be involved in. CMA asked members of the PPG to complete a brief questionnaire about how they usually booked appointments and advised that this would contribute to the partnership’s information gathering. CMA also asked members of the PPG to have positive conversations with patients who may say that it is challenging to get appointments, or are experiencing problems getting through on the phones.
Any other business
Wendy Jones (WJ) advised members that she had recently undertaken a project knitting hats for elderly people who were in hospital or had recently had surgery. The hospital had expressed their thanks for this and this was something WJ was keen to continue. To support with this, WJ asked members if they could let her have any wool that they may have spare.
Action: Members to donate wool to WJ for her hats for the elderly project. Representatives from MVMP can leave these at Moss Valley and CMA will take them to GVMP for WJ.
Date of next meetings
The next meeting of the PPG was confirmed as Thursday 19 September 2024 from 18:30 at Gosforth Valley Medical Practice. The Chair said that Rhonda Pickering, from DHU would like to come along as our guest speaker.
